Imagine living in a constant loop of unwanted thoughts, accompanied by an unrelenting urge to perform certain actions to alleviate them. For individuals with Obsessive-Compulsive Disorder (OCD), this is a daily reality. OCD is more than just a preference for neatness or a desire for organization—it’s a chronic mental health condition marked by intense anxiety, distressing obsessions, and repetitive compulsions. Navigating life with OCD can be exhausting and confusing, but understanding the condition is a crucial first step toward compassion, empowerment, and effective treatment.
What Is OCD?
Obsessive-Compulsive Disorder is a mental illness that involves two main symptoms: obsessions and compulsions.
Obsessions are intrusive and unwanted thoughts, images, or urges that trigger significant anxiety or discomfort. These are not just worries or thoughts one can easily dismiss—they are persistent and often disturb the person experiencing them. Common obsessions include fear of contamination, concerns about safety, a need for symmetry or order, or disturbing taboo thoughts.
Compulsions are behaviors or mental acts performed in response to an obsession. These acts are meant to reduce the distress or prevent a feared outcome. Examples include excessive handwashing, repeated checking, counting, praying, or seeking reassurance. Although compulsions might temporarily ease anxiety, they reinforce the cycle of OCD and can dominate a person’s daily life.
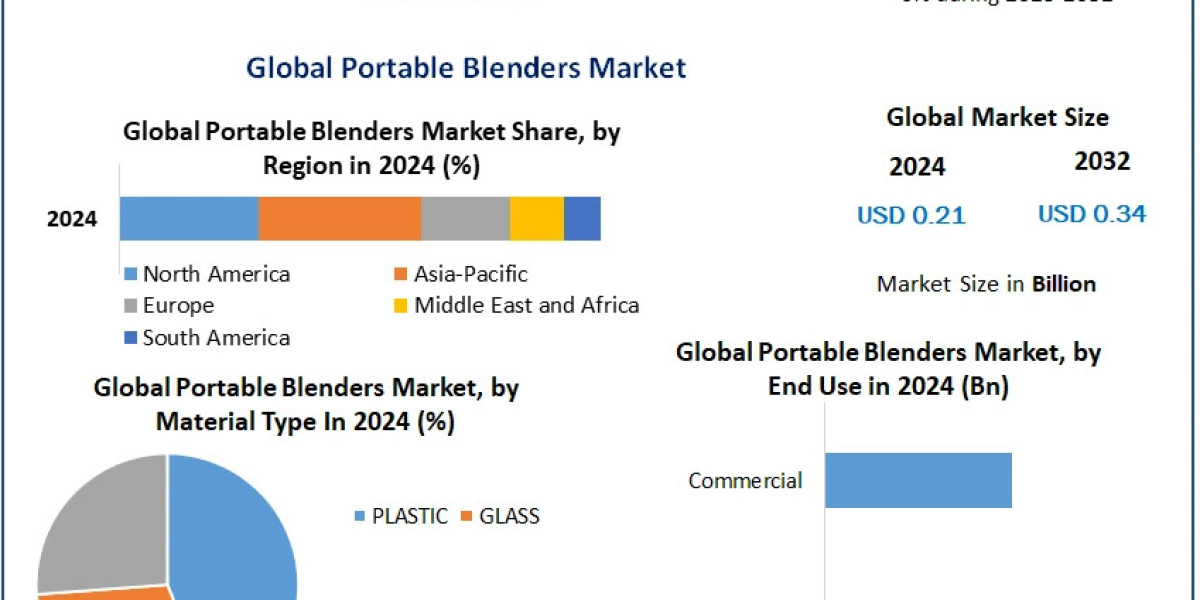
OCD is not simply being "quirky" or "perfectionistic." It’s a serious disorder that affects about 2–3% of the global population. It can interfere with work, relationships, education, and overall quality of life.
The Cycle of OCD
Understanding the OCD cycle is key to recognizing the disorder and seeking appropriate help. The cycle typically follows this pattern:
Trigger – A situation or internal thought that initiates the obsessive fear.
Obsession – The disturbing thought or image appears and creates anxiety.
Anxiety – The person feels overwhelming distress or fear.
Compulsion – A behavior or mental ritual is performed to reduce anxiety.
Temporary Relief – The compulsion reduces the anxiety, reinforcing the behavior.
Cycle Repeats – Obsession returns, and the cycle begins again.
For many, this cycle can dominate hours of their day and create emotional and physical exhaustion. The relief offered by compulsions is short-lived, making the behavior repetitive and difficult to resist.
Living with OCD: The Hidden Struggle
One of the hardest parts of living with OCD is how misunderstood it often is. While some symptoms are visible—like checking a door lock repeatedly—others are more internal and harder to detect. Many people with OCD suffer in silence, feeling ashamed or confused by their thoughts and behaviors. They may fear being judged or not taken seriously, especially when their compulsions appear irrational to others.
Additionally, OCD can co-occur with other mental health conditions like depression, anxiety disorders, eating disorders, or tic disorders. This overlap can complicate diagnosis and treatment, making it even more essential to seek professional help.
Myths and Misconceptions
Myth 1: OCD is just about being neat or organized.
Truth: OCD can involve cleanliness, but it’s much broader. Obsessions can be about morality, harm, or even existential fears, and not all compulsions are related to order.
Myth 2: People with OCD can stop their behaviors if they really want to.
Truth: OCD is not a matter of willpower. The compulsions are driven by intense anxiety and an urgent need to relieve distress. Stopping them without help can feel nearly impossible.
Myth 3: OCD is rare.
Truth: OCD is fairly common and affects people of all ages and backgrounds. It often begins in childhood or adolescence and can persist into adulthood if untreated.
Diagnosis and Treatment
OCD is typically diagnosed by a psychologist or psychiatrist through a comprehensive assessment of symptoms. A proper diagnosis often leads to effective treatment, which can dramatically improve quality of life.
The most effective treatments for OCD include:
Cognitive Behavioral Therapy (CBT), especially Exposure and Response Prevention (ERP): This therapy helps individuals confront their fears and resist the urge to perform compulsions. Over time, anxiety decreases, and the compulsive behavior loses its power.
Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) are commonly prescribed to help manage OCD symptoms. They can reduce the frequency and intensity of obsessions and compulsions.
Mindfulness and Acceptance Strategies: These approaches teach people to tolerate intrusive thoughts without reacting to them, which can help weaken the OCD cycle.
Support Systems: Peer support groups, family therapy, and education can also be powerful tools in helping individuals with OCD feel less alone and more understood.
Navigating Daily Life with OCD
For someone living with OCD, everyday activities can feel like a minefield. Simple tasks like turning off the stove, shaking someone’s hand, or sending an email might spiral into hours of obsessive thinking and compulsive behavior.
However, many people with OCD lead full and successful lives once they learn to manage their symptoms. Navigating OCD is a journey, often marked by setbacks and progress. Patience, persistence, and professional support are key.
Building healthy routines, practicing self-compassion, and learning to accept uncertainty can make a significant difference. Avoiding compulsions may initially increase anxiety, but with practice and support, most individuals experience relief and a sense of control.
Final Thoughts
Obsessive-Compulsive Disorder is a complex and often misunderstood condition, but it is also highly treatable. By educating ourselves and others, we can break the stigma and support those who are silently struggling.
OCD does not define a person. It’s one part of their story—but with the right help, tools, and understanding, it’s a chapter that can be rewritten with hope, strength, and resilience.